There are times when physicians order special diets for their clients for different reasons, such as disease, weight control, or physical or neurological changes that put clients at risk of choking. But just like any meal planning, the client’s preferences, culture, religion, allergies, and intolerances are taken into consideration.
In care facilities, when a client does not have any dietary restrictions, their diet would be called either a regular or general diet. However, there are many types of special diets that you may see in your practice. For example, there are restricted diets, such as the diabetic diet, sodium-controlled diet, or a gluten-free diet. There are also diets that have modified texture due to illness, disease, or neurological and physical disabilities. A clear-liquid diet would be for acute illness or for post-operative patients, or the mechanical soft diet may be used for gastro-intestinal disorder, or moving from a liquid diet. Whatever diet is ordered for the client, it is chosen based on a thorough assessment of the client’s history, health status, and ability to swallow, and it will be outlined in their care plan.
Considerations
- If the client has facial weakness, arm/hand weakness, or paralysis, assist with eating from the client’s strong side and place eating utensils on their stronger side.
- If the client has a swallowing problem, allow longer periods between bites for adequate chewing and swallowing. Encourage the client to tuck their chin down and bend their body forward while swallowing. This encourages the food to move down the esophagus.
- Limit the amount of conversation while the client is chewing and/or swallowing.
- Ensure that food is cut into bite-sized pieces and that food is the appropriate consistency (e.g., pureed), according to the client’s prescribed diet.
Types of Modified Texture Diets

Table 6.4.1: Liquid Consistencies
| LEVEL | TYPE | DESCRIPTION/ CHARACTERISTICS |
| 0 | Thin drinks |
|
| 1 | Slightly Thick drinks |
|
| 2 | ‘Sippable’ drinks |
|
| 3 | Moderately thick drinks |
|
| (Source: IDDSI, 2019) CC BY SA 4.0 | ||
Adaptive eating devices are modified utensils, dishes, and cups to make it easier for people with different types of physical difficulties to eat — clients who may be weak or have difficulty grasping utensils. These devices can enhance mealtime and client independence, as well. While there are many such devices on the market, they can easily be made by simply building up the hand of eating utensils with gauze and tape.

Special Diets – Enteral Nutrition
Some clients, because of illness, injury, or surgery, have extreme difficulty chewing or swallowing and as a result have additional dietary considerations. For such clients, it is unsafe to eat or drink by mouth, therefore a physician will order all foods, fluids, and medications to be given through a tube. Only licensed healthcare workers can administer the foods, fluids, and medications through the tube, but as an HCA you will care for clients who have had these procedures, so it is important for you to understand.
Enteral nutrition is provided to people who cannot chew or swallow foods or fluids past their esophagus into their stomachs. Enteral nutrition is a liquid nutritional formula delivered into the gastro-intestinal tract through a Gavage tube. The need for enteral nutrition may occur due to trauma or cancers to the face, mouth, esophagus, or neck. Also, people with advanced dementia who no longer know how to eat may have a gavage tube. Many people refer to these types of tubes as “G-tubes,” and there are many types of G-tubes depending on where they are surgically placed (Sorrentino, et al., 2019).
Table 6.4.2: Types of Enteral Nutritional Feeding Tubes
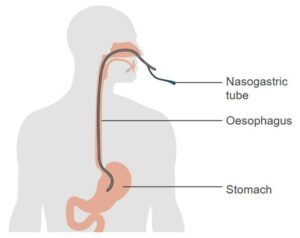
| Nasogastric (NG) tube:
Inserted through the nose into the stomach |
 |
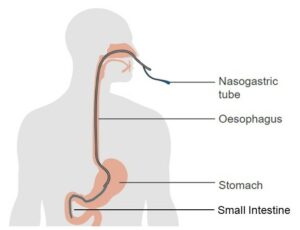
| Naso-intestinal (NG) tube:
Inserted through the nose into the small intestine |
 |
| Gastrostomy (G-tube) tube:
Inserted directly into the stomach through surgical opening. Types of tubes include the J-tube and the PEG-tube as noted below. |
 |
| Jejunostomy (J-tube) tube or Gastro-jejunostomy (GJ) tube:
Placed in surgical opening in middle of small intestine (jejunum). Access is both stomach and jejunum. Typically, the tube is placed in a G-tube stoma with a narrower long tube into the small intestine. Used with clients at high risk of aspiration. |
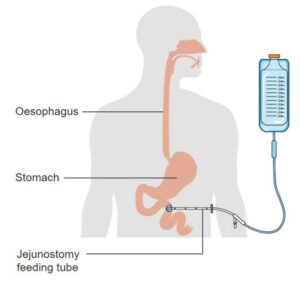 |
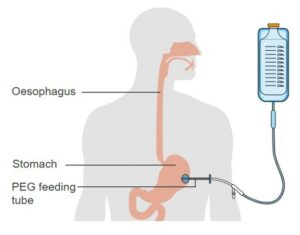
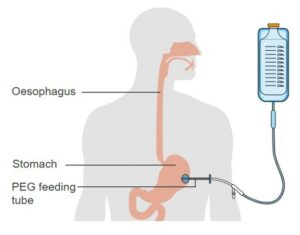
| Percutaneous endoscopic gastrostomy (PEG) tube:
Using an endoscope to see into the stomach, the physician will make a puncture wound (stomy) in the skin and into the stomach. A short tube is inserted into the stomach through the puncture wound and the tube sits flush against the skin.
|
 |
(Source: Sorrentino, et al., 2019)
How often a client may receive enteral nutrition depends on how the physician or dietician orders them, as well as the type of tube in place. There could be scheduled feedings given four times per day or these could be continuous over the day. Naso-intestinal and jejunostomy tube feedings are always continuous.
What is the HCA Role in Enteral Nutrition?
As the HCA care for someone with an enteral feeding tube your role mostly be observation, unless the task has been delegated to you by a licensed healthcare worker at your agency. Clients with enteral feeding tubes are at risk for aspiration. These tubes can move from the stomach or intestine and into the esophagus or airway because clients move, or they or their caregivers may accidentally pull on the tube. Also, with such tubes regurgitation may occur due to delayed stomach emptying and over-feeding. To prevent regurgitation and aspiration, have the client in a semi-Fowler’s or sitting position during feeding and for at least one hour after eating to promote digestion. Also, avoid putting the client in a left-lying side position as this prevents stomach emptying.
Observations and Comfort Measures
As the HCA caring for clients with enteral feeding tubes, it is essential you use your skills to make observations and provide comfort because aspiration is not the only risk with this type of feeding. Delayed stomach emptying, diarrhea, and constipation can also occur, so observe and report any of the following immediately to your supervisor:
- Coughing or gurgling voice
- Nausea, vomiting
- Diarrhea
- Discomfort during the tube feeding
- Stomach distention (enlarged or swollen)
- Elevated temperature and/or pulse rate
- Redness, swelling, drainage, odour, pain at ostomy site
Because most people with enteral feeding tubes do not take anything by mouth (NPO), mouth care is extremely important. Dry mouth and lips and sore throat can cause discomfort; therefore, good oral hygiene will be required. Brush teeth, moisturize lips and mouth, and if allowed, offer ice chips or hard candy to suck on. If the tube is placed into the nose, the tubes can put pressure on the nose and it becomes irritated and red. Try to reposition the tube slightly away from the nostril; tape or tube holders can be used to help with this and be sure to clean the nose at least every four hours. To prevent the tube from being pulled out of place, pin or secure the tubing to the client’s gown with a rubber band and safety pin or secure-strip with enough slack to allow movement.
Measuring Intake
To maintain adequate health, individuals need to take in a certain amount of fluid per day. Depending on a client’s condition, they may either be encouraged to drink fluids or limit their fluid intake. Fluid that is taken in is called intake. Fluids are usually measured using milliliters (ml). One cup of liquid is 8 ounces or 250 ml.
The amount of food that is eaten can also be measured. This can be done by weighing the food prior to serving and subtracting the amount left to get the total food intake. Food intake can also be measured by determining the total percentage eaten. If all the meal is consumed, the intake is 100%. If none of the meal is consumed, the intake is 0%. A quarter of the meal consumed would be 25% and half the meal consumed would be 50% (McLain, et al., 2018; Sorrentino, et al., 2019). The facility policy will specify the unit of measurement to be used.
- ⇒ Explain to the client the importance of recording their intake. Throughout your shift, monitor or ask the client what and how much they have had to eat or drink.
- ⇒ During food preparation, measure the amount of food or liquid that is served. Use standard measuring cups and spoons to properly measure intake. Record this in the appropriate place.
- ⇒ Once the client has finished eating or drinking, subtract the amount they have consumed from the amount you served. Record this number as their input. Input for fluid should be recorded as millitres (ml).
- ⇒ Record the weight or percentage of food consumed in the appropriate place.
- ⇒ Document all food and drink intake. The agency may provide a specific intake and output (I & O) sheet. Healthcare staff including HCAs should report any observations or changes in condition or behavior.
Learning Activity
Complete this Meal Assistance Virtual Game Simulation Activity by Hughes, Kenmir, & Romaniuk ( n.d.).
When you have completed this, answer the reflective questions and complete the “Test Your Knowledge” quiz found at the end of this activity.
Summary:
There are many factors that affect individuals’ eating and nutrition. Factors such as culture, religion, age, illness, and disability to name a few. It is important to understand your clients’ preferences and needs by getting to know them and following the care plan. It is also important to know who is at risk of choking, and how the HCA can prevent such situations. Following the care plan is especially important when assisting a client to eat and knowing how to record and report the intake of foods and fluids.
Chapter 6 Attributions and References
Unit 6.2 Image Attributions
- Figure 6.2.1 Illu conducting passages (https://commons.wikimedia.org/wiki/File:Illu_conducting_passages.svg) [adapted], by Jmarchn, via Wikimedia Commons, is in the public domain (https://en.wikipedia.org/wiki/en:Public_domain). [Vectorized version of File:Illu conducting passages.jpg, which was a work of the US Government. Originally from SEER Training, U.S. National Cancer Institute (https://training.seer.cancer.gov/anatomy/respiratory/passages/).]
- http://cnx.org/content/col11496/1.6/, Jun 19, 2013., CC BY 3.0, https://commons. wikimedia.org/w/index.php?curid=30148430
- Figure 6.2.2. Real-time MRI – Swallowing (Pineapple Juice) (https://commons.wikimedia.org/wiki/File:Real-time_MRI_-_Swallowing_(Pineapple_Juice).ogv) by Biomedizinische NMR Forschungs GmbH (https://www.mpinat.mpg.de/en/frahm/), via Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/deed.en) licence.
Unit 6.4 Image Attributions
- Figure 6.4.1 Textures-Modified Diets (https://iddsi.org/United-Kingdom) © The International Dysphagia Diet Standardisation Initiative 2019. This infographic is used under a CC BY SA 4.0 Derivative works extending beyond language translation are NOT PERMITTED.
- Figure 6.4.2 Adaptive Utensils by AMorice CC0
- Figure 6.4.3 Diagram showing the position of a nasogastric tube CRUK 340 (https://commons.wikimedia.org/wiki/File:Diagram_showing_the_position_of_a_nasogastric_tube_CRUK_340.svg) by Cancer Research UK, via Wikimedia Commons, is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0/deed.en) licence.
- Figure 6.4.4 [adapted] Diagram showing the position of a nasogastric tube CRUK 340 (https://commons.wikimedia.org/wiki/File:Diagram_showing_the_position_of_a_nasogastric_tube_CRUK_340.svg) by Cancer Research UK, via Wikimedia Commons, is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0/deed.en) licence.
- Figure 6.4.5 Diagram showing the position of a percutaneous endoscopic gastrostomy (PEG) feeding tube CRUK 341 (https://commons.wikimedia.org/wiki/File:Diagram_showing_the_position_of_a_percutaneous_endoscopic_gastrostomy_%28PEG%29_feeding_tube_CRUK_341.svg) by Cancer Research UK, via Wikimedia Commons, is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0/deed.en) licence.
- Figure 6.4.6 Diagram showing the position of a percutaneous jejunostomy feeding tube CRUK 342 (https://commons.wikimedia.org/wiki/File:Diagram_showing_the_position_of_a_percutaneous_jejunostomy_feeding_tube_CRUK_342.svg) by Cancer Research UK, via Wikimedia Commons, is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0/deed.en) licence.
- Figure 6.4.7 Diagram showing the position of a percutaneous endoscopic gastrostomy (PEG) feeding tube CRUK 341.svg (https://commons.wikimedia.org/wiki/File:Diagram_showing_the_position_of_a_percutaneous_endoscopic_gastrostomy_(PEG)_feeding_tube_CRUK_341.svg) by Cancer Research UK, via Wikimedia Commons, is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0/deed.en) licence.
- Table 6.4.1 Liquid Consistencies The International Dysphagia Diet Standardisation Initiative. (2019). IDDSI Testing Method – English (pdf, July 2019)
- Table 6.4.2 Types of Enteral Nutritional Feeding Tubes (Sorrentino, et al., 2019).
Videos
- Feed a Resident in a Chair CNA Skill NEW! (https://www.youtube.com/watch?v=uA5V-ivcEes) by 4yourCNA (2016) on YouTube.
- PEARSON VUE/CREDENTIA 2022 – FEEDS CLIENT WHO CANNOT FEED SELF (https://www.youtube.com/watch?v=faw_mOmoDxk) by Nurse Jar (2019), on YouTube.
- Understanding Dysphagia (https://www.youtube.com/watch?v=jK1o3LSQmB0) by Nestlé Health Science Canada (2011), on YouTube.
References
4yourCNA [username]. (2016, August 4). Feed a resident in a chair CNA Skill NEW! (Video). YouTube. https://www.youtube.com/watch?v=uA5V-ivcEes
Girdi-Papp, M. (2022). Comparative Oral+ENT Biology. Comparative Oral+ENT Biology : Marcos Gridi-Papp : Free Download, Borrow, and Streaming : Internet Archive . Chpt 20 pg 438–450. This book is licensed under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/) licence.
Hughes, M., Kenmir, A., Romaniuk, D., & Vander Meeren, P. (n.d.). Meal assistance virtual gaming simulation – Simple book publishing. ECampus Ontario. https://ecampusontario.pressbooks.pub/mavgs/
International Dysphagia Diet Standardisation Initiative (IDDSI). (2019, July). Complete IDDSI Framework
Detailed definitions 2.0 | 2019 [IPDF]. https://iddsi.org/IDDSI/media/images/Complete_IDDSI_Framework_Final_31July2019.pdf. This work is used under a CC BY SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0/legalcode) license. Derivative works extending beyond language translation are NOT PERMITTED.
International Dysphagia Diet Standardisation Initiative (IDDSI). (2022, September). Textured Modified diets [Infographic/PDF]. UK IDDSI Reference Group (UKIRG). https://iddsi.org/IDDSI/media/images/CountrySpecific/UnitedKingdom/Texture-Modified-Diets-(UK-IDDSI-Festival).png. This work is used under a CC BY SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0/legalcode) license. [Developed with Four Seasons Health Care.] Derivative works extending beyond language translation are NOT PERMITTED.
McLain, K., O’Hara-Leslie, E., & Wade, A. (n.d.). Foundations for assisting in home care. Milne Publishing/SUNY Geneseo. https://milnepublishing.geneseo.edu/home-health-aide/ This book is licensed under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/) licence.
Nestlé Health Science Canada. (2011, May 11). Understanding Dysphagia (Video). YouTube. https://www.youtube.com/watch?v=jK1o3LSQmB0
Nurse Jar. (2019, April 13). PEARSON VUE/CREDENTIA 2022 – FEEDS CLIENT WHO CANNOT FEED SELF (Video). YouTube. https://www.youtube.com/watch?v=faw_mOmoDxk
Sorrentino, S., Remmert, L., & Wilks, M. (2019). Mosby’s Canadian textbook for the support worker (4th ed.). Elsevier Canada.
Biomedizinische NMR Forschungs GmbH. (2011, September 16). Real-time magnetic resonance imaging at a resolution of 20 ms [GIF]. Wikimedia Commons. https://commons.wikimedia.org/wiki/File:Real-time_MRI_-_Swallowing_(Pineapple_Juice).ogv
Feeding tube
Inhalation of fluids or object into the lungs
Backward flow of food/fluid from the stomach into the mouth
do not take anything by mouth

