What is Temperature?
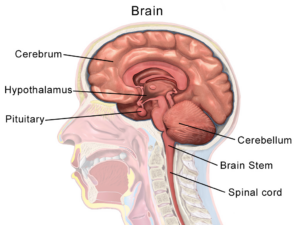
Temperature refers to the degree of heat or cold in an object or a human body. In humans, the brain’s hypothalamus acts as the body’s thermostat and is responsible for regulating its temperature. See Figure 9.5.1 of the hypothalamus.
The human body is constantly adapting to internal health states and environmental conditions, and the hypothalamus is programmed to tell the body to generate heat if the body temperature is low. For example, the hypothalamus can activate peripheral vasoconstriction and shivering (contraction of skeletal muscles) to prevent a decrease in body temperature. The hypothalamus can also reduce heat if the body temperature is too high. For example, it can activate peripheral vasodilation to increase heat loss and cause a person to perspire, which cools the body.
Why is Temperature Measured?
Healthcare providers measure a client’s temperature because it can give information about their state of health and influence clinical decisions. Accurate measurements and interpretation are vital so that hyperthermia and hypothermia can be identified and appropriate interventions determined.
Hyperthermia refers to an elevated body temperature. It can be related to an internal or external source. External sources that increase body temperature could include exposure to excessive heat on a hot day or being in a sauna or hot tub. Internal sources that may increase body temperature include fever caused by an infection or tissue breakdown associated with physical trauma (e.g., surgery, myocardial infarction) or some neurological conditions (e.g., cerebral vascular accident, cerebral edema, brain tumour). Hyperthermia that is associated with an infectious agent, such as a bacteria or virus (e.g., the flu) is referred to as febrile. Unresolved hyperthermic body states can lead to cell damage.
Hypothermia refers to a lowered body temperature. It is usually related to an external source such as being exposed to the cold for an extended period of time. Hypothermia is sometimes purposefully induced during surgery, or for certain medical conditions, to reduce the body’s need for oxygen. Unresolved hypothermic body states can slow cellular processes and lead to loss of consciousness.
Methods of Measurement
Methods of measuring a client’s body temperature vary based on developmental age, cognitive functioning, level of consciousness, state of health, safety, and agency/unit policy. The LPN /RN will choose the best method after considering client safety, accuracy, and least invasiveness, all contingent on the client’s health and illness state. The most accurate way to measure core body temperature is an invasive method through a pulmonary artery catheter. This is only performed in a critical care area when constant measurements are required along with other life-saving interventions.
Methods of measurement include oral, axillary, tympanic, rectal, and dermal routes.
Oral temperature can be taken with clients who can follow instructions, so this kind of measurement is common for clients over the age of four, or even younger children if they are cooperative. Another route other than oral (e.g., tympanic or axillary) is preferable when a client is on oxygen delivered via a face mask because this can alter the temperature.
For children younger than four, axillary temperature is commonly measured unless a more accurate reading is required.
Rectal temperature is an accurate way to measure body temperature (Mazerolle, Ganio, Casa, Vingren, & Klau, 2011). The rectal route is recommended by the Canadian Pediatric Society for children under two years of age (Leduc & Woods, 2017). However, this method is not used on infants younger than thirty days or premature infants because of the risk of rectal tearing. If the rectal method is required, the procedure is generally only used by nurses and physicians.
Dermal routes are alternative methods of measurement that may be used in some agencies and practice areas. This method can involve holding the device and sliding it over the skin of the forehead and then down over the temporal artery in one motion. Dermal strips can also be placed on the forehead to measure skin temperature, but are not yet widely used, and the accuracy of this method has not yet been verified. More recently, there has been an increase in non-contact infrared thermometers particularly in the era of COVID-19 and other highly transmissible diseases. Depending on the type, these thermometers can be held at a short distance from the forehead or temporal area to measure temperature. Alternatively, some handheld thermal scanners that use an infrared camera can be held at a greater distance to screen large masses of people. Please refer to the manufacturer’s suggested reference range for non-contact infrared thermometers and thermal scanners.
What are Normal Temperature Ranges?
The human body’s core temperature (internal body temperature) is measured in degrees Celsius (ºC) or Fahrenheit (ºF). In Canada, degrees Celsius is most commonly used.
In adults, the normal core body temperature (referred to as normothermia or afebrile) is 36.5–37.5ºC or 97.7–99.5ºF.
A wider temperature range is acceptable in infants and young children, and can range from 35.5–37.7ºC or 95.9–99.8ºF. Infants and children have a wider temperature range because their heat control mechanisms are less effective. They are at risk for heat loss for many reasons including having less subcutaneous fat than adults, a larger body surface area in comparison to weight (and larger head size in proportion to the rest of the body), immature metabolic mechanisms (e.g., they may be unable to shiver), and limited ability to produce heat through activity. They are also at risk of excessive heat production due to crying and restlessness as well as external factors such as being wrapped in too many blankets.
Older adults tend to have lower body temperatures and are at risk for hypothermic states; reasons for this may include having less subcutaneous tissue acting as insulation, loss of peripheral vasoconstriction capacity, decreased cardiac output with resultant lowered blood flow to the extremities, decreased muscle mass resulting in reduced heat production capacity, and decreased metabolic responses.
See Table 9.6.1 for normal temperature ranges based on method. The normal ranges vary slightly for each of the methods. It is important to consider a client’s baseline temperature as some individuals present with a temperature slightly above or below these ranges. It is not the Health Care Assistant’s role to make a clinical judgement about the temperature measurement; this is the responsibility of the LPN or RN.
Table 9.6.1: Normal Temperature Ranges
|
Method |
Range |
| Oral | 35.8–37.3ºC |
| Axillary | 34.8–36.3ºC |
| Tympanic | 36.1–37.9ºC |
| Rectal | 36.8–38.2ºC |
Other factors that influence temperature include diurnal rhythm, exercise, stress, menstrual cycle, and pregnancy. The diurnal cycle causes a fluctuation of 1ºC, with temperatures lowest in the early morning and highest in the late afternoon. During exercise, body temperature rises because the body is using energy to power the muscles. Temperature can rise as a result of stress and anxiety, due to stimulation of the sympathetic nervous system and increased secretion of epinephrine and norepinephrine. Body temperature varies throughout a woman’s menstrual cycle due to hormonal fluctuations, rising after ovulation until menstruation by about 0.5–1ºC. Body temperature is slightly elevated during pregnancy as a result of increased metabolism and hormone production such as progesterone.
Oral Temperature
The normal oral temperature is 35.8–37.3ºC or 96.4–99.1ºF. Oral temperature measurement is common and reliable because it is close to the sublingual artery. An oral thermometer is shown in Figure 9.6.2. The device has blue colouring, indicating that it is an oral or axillary thermometer as opposed to a rectal thermometer, which has red colouring.

Technique
Remove the probe from the device and place a probe cover (from the box) on the oral thermometer without touching the probe cover with your hands. Place the thermometer in the client’s mouth under the tongue and instruct client to keep mouth closed and not to bite on the thermometer. Ensure the thermometer probe is in the posterior sublingual pocket under the tongue, slightly off-centre. Leave the thermometer in place for as long as is indicated by the device manufacturer. The thermometer will beep within a few seconds when the temperature has been taken: most oral thermometers are electronic and provide a digital display of the reading. Discard the probe cover in the garbage (without touching the cover) and place the probe back into the device. See Figure 9.6.3 of an oral temperature being taken.

What should the Health Care Assistant consider?
Health Care Assistants often measure the oral temperature, particularly when the client is conscious and can follow directions. Measurement of the oral temperature is not recommended for individuals who are unconscious, unresponsive, confused, have an endotracheal tube secured in the mouth, and cannot follow instructions.
Certain factors render the oral route less accurate with the potential for falsely high or falsely low findings. If the client has recently consumed hot or cold food or beverage, chewing gum, or has smoked prior to measurement, the healthcare provider should use another route such as tympanic or axillary. Selecting an alternate route under the aforementioned circumstances is most conducive to a fast-paced clinical environment and most respectful of the client’s time. If another route is not available, healthcare providers should wait 15 to 25 minutes to take the oral temperature following consumption of a hot or cold beverage/food. The temperature of the beverage/food also factors into the wait period, as extreme heat or cold will require longer wait times for oral temperature assessment. Health Care Assistants should wait about 5 minutes if the client is chewing gum or has just smoked since both of these activities can increase temperature.
Watch this YouTube video showing how to take an Oral Temperature
Test Yourself!
While watching the interactive video on measuring temperature with an oral thermometer, apply your knowledge and critical thinking skills to answer the questions throughout the video. Please note: there is no sound in this video.
Tympanic Temperature
The normal tympanic temperature is usually 0.3–0.6°C higher than an oral temperature. It is accurate because the tympanic membrane shares the same vascular artery that perfuses the hypothalamus. A tympanic thermometer is shown in Figure 9.6.4.

Technique
Remove the tympanic thermometer from the casing and place a probe cover (from the box) on the thermometer tip without touching the probe cover with your hands. Only touch the edge of the probe cover (if needed), to maintain clean technique. Turn the device on. Ask the client to keep head still. For an adult or older child, gently pull the helix up and back to visualize the ear canal. For an infant or younger child (under 3), gently pull the lobe down. The probe is inserted just inside the opening of the ear. Never force the thermometer into the ear and do not occlude the ear canal. Only the tip of the probe is inserted in the opening – this is important to prevent damage to the ear canal. Activate the device; it will beep within a few seconds to signal it is done. Discard the probe cover in the garbage (without touching the cover) and place the device back into the holder. See Figure 9.6.5 of a tympanic temperature being taken.

Technique Tips
The technique of pulling the helix up and back (adult) or the lobe down (child under 3) is used to straighten the ear canal so the light can reflect on the tympanic membrane. If this is not correctly done, the reading may not be accurate. The probe tip is gently inserted into the opening to prevent damage to the ear canal. The ear canal is a sensitive and a highly innervated part of the body, so it is important not to force the tympanic probe into the ear.
What should the Health Care Assistant consider?
The tympanic temperature method is a quick and minimally invasive way to take temperature. Although research has proven the accuracy of this method, some pediatric institutions prefer the accuracy of the rectal temperature. The Canadian Pediatric Society found equal evidence for and against the use of tympanic temperature route (Leduc & Woods, 2017). It concluded that tympanic temperature is one option for use with children, but suggested using rectal temperature for children younger than two, particularly when accuracy is vital. The tympanic temperature is not measured when a client has a suspected ear infection. It is important to check your agency policy regarding tympanic temperature.
Watch this YouTube video showing how to take a Tympanic Temperature
Test Yourself!
While watching the interactive video on measuring temperature with a tympanic thermometer, apply your knowledge and critical thinking skills to answer the questions throughout the video. Please note: there is no sound in this video.
Axillary Temperature
The normal axillary temperature may be as much as 1ºC lower than the oral temperature. An axillary thermometer is the same electronic device as an oral thermometer, and both have a blue end.
Technique

Remove the probe from the device and place a probe cover (from the box) on the thermometer without touching the cover with your hands. Ask the client to raise the arm away from his/her body. Place the thermometer in the client’s armpit, on bare skin, as high up into the axilla as possible, with the point facing behind the client. Ask the client to lower his/her arm and leave the device in place for as long as is indicated by the device manufacturer. Usually the device beeps in 10–20 seconds. Discard the probe cover in the garbage (without touching the cover) and place the probe back into the device. See Figure 9.6.6 of an axillary temperature being taken.
What should the Health Care Assistant consider?
The axillary route is a minimally invasive way to measure temperature. It is commonly used in children. It is important to ensure that the thermometer is as high up in the axilla as possible with full skin contact and that the client’s arm is then lowered down.
Watch this YouTube video showing how to take an Axillary Temperature
Test Yourself!
While watching the interactive video on measuring temperature with an axillary thermometer, apply your knowledge and critical thinking skills to answer the questions throughout the video. Please note: there is no sound in this video.
Rectal Temperature
The normal rectal temperature is usually 1ºC higher than oral temperature. A rectal thermometer has a red end to distinguish it from an oral/axillary thermometer. A rectal thermometer is shown in Figure 9.6.7.

Technique
First, ensure the client’s privacy. Wash your hands and put on gloves. For infants, lie them down in a supine position and raise their legs up toward the chest. You can encourage a parent to hold the infant to decrease movement and provide a sense of safety. With older children and adults, assist them into a side lying position. Remove the probe from the device and place a probe cover (from the box) on the thermometer. Lubricate the cover with a water-based lubricant, and then gently insert the probe 2–3 cm inside the rectal opening of an adult, or less depending on the size of the client. The device beeps when it is done.
What should the Health Care Assistant consider?
Measuring rectal temperature is an invasive method. Some suggest its use only when other methods are not available, while others suggest that the rectal route is a gold standard in the infant population because of its accuracy. The Canadian Pediatric Society (Leduc & Woods, 2017) has referred to research indicating that rectal temperatures may remain elevated after a client’s core temperature has started to return to normal, but after reviewing all available evidence, still recommends measuring rectal temperature for children under the age of two, particularly when accuracy is vital. Rectal temperature is not measured in infants under one month of age or premature newborns.
Summary
Temperature is an important vital sign because it provides current data about the client’s health and illness state. Changes in body temperature act as a cue for healthcare providers’ diagnostic reasoning.
There are many ways to measure temperature. In determining the best method, the LPN/RN considers agency policy, the client’s age and health and illness state, and the reason for taking the temperature. Health Care Assistants must use the correct technique when measuring temperature, because this can influence client data.
The role of the Health Care Assistant is limited to measuring temperature. The LPN/RN will determine the relevance of the temperature, and consider the client’s baseline data and the situation. Diagnostic reasoning about temperature always involves considering additional data including other vital sign measurements and subjective and objective client data.
Exercises

